
Dementia: Engaging the Mind and Body By: Jillian Lisiakowski, DNP, FNP-C, ACHPN
January 23, 2025
Myth Buster 1
February 17, 2025Symptom Series: Dyspnea
By: Jillian Lisiakowski, DNP, FNP-C, ACHPN
Many common symptoms are experienced at the end of life, including nausea, dyspnea, pain, loss of appetite, weakness, and confusion. Dyspnea, or shortness of breath, can lead to anxiety, discomfort, and reduced activity, all leading to decreased quality of life. Symptoms such as dyspnea can be distressing, but a trained hospice and palliative care team can often manage them effectively at home. Treatment for dyspnea may involve both pharmaceutical and non-pharmaceutical therapies and can lead to an increased quality of life for the patient.
What is Dyspnea?
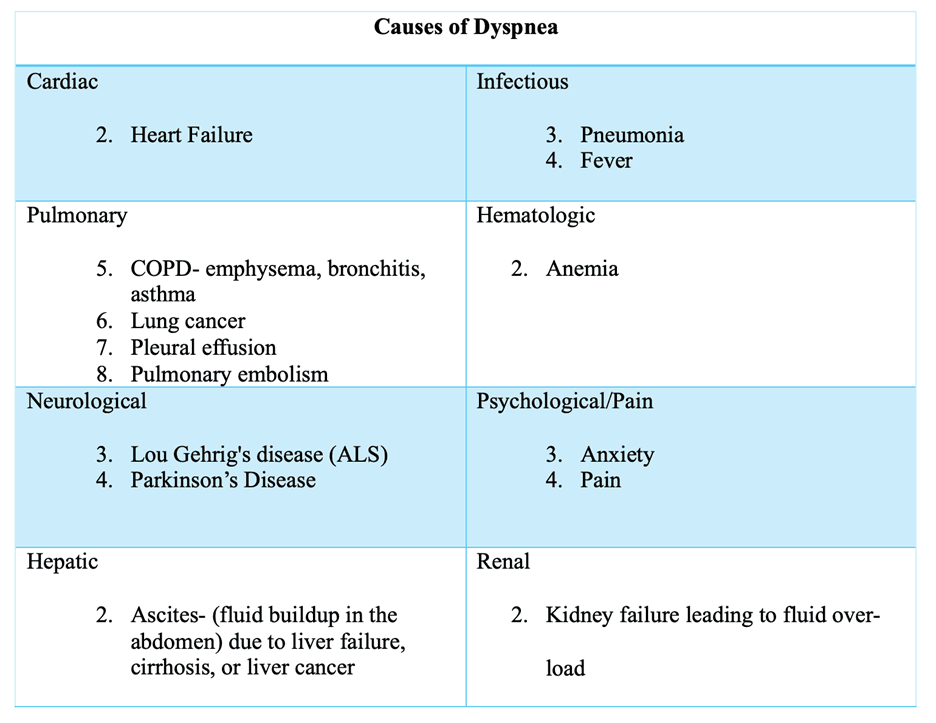
Dyspnea is defined as the experience of breathing discomfort that can vary in intensity and have cause physical, psychological, emotional, and social implications. Dyspnea is similar to pain and nausea in that it is a symptom that can only be described by the patient. There are many causes of dyspnea, including cardiac, infectious, pulmonary, hematologic, neurologic, hepatic, and renal disorders. Examples of the different causes of dyspnea are listed below. Treatment for each type of dyspnea can vary based on the cause and include non-pharmacological therapies.
Treatment options
The treatment of dyspnea will vary based on the suspected cause. Low doses of opioid medications are often used to treat dyspnea as they can reduce pain and allow for more substantial inhalation and exhalation. Diuretics, commonly known as water pills, such as furosemide and spironolactone, can assist with dyspnea by helping to rid the body of extra fluid that may impair breathing. Supplemental oxygen may also be ordered if the patient’s dyspnea is related to low oxygen levels. Other medications, such as benzodiazepines, help to reduce feelings of anxiety and lead to reduced feelings of dyspnea.
In addition to medication, it is important to assess and address the causes of psychosocial, spiritual, and emotional distress. Social workers and chaplains on the hospice team are often well-equipped to listen and lead individual or group conversations that may help resolve or address unspoken concerns. As these concerns are resolved, many patients feel like they are able to breathe more easily. Maintaining a peaceful and calm environment may also help reduce feelings of dyspnea. Cooling the room or placing a fan facing toward the patient has also been known to relieve dyspnea.
While dyspnea can be scary and frustrating, working with the hospice care team can reduce symptoms and improve quality of life. Several types of therapies may be needed to control feelings of dyspnea adequately. For example, low-dose opioids and a fan may be used jointly. Try to remain open-minded to utilizing both pharmaceutical and non-pharmaceutical therapies to manage dyspnea and communicate what works best with your healthcare team. The hospice and palliative care team is ready to work with you to ensure symptoms are managed and well-controlled in the home.
References
Dahlin, C., & And, H. (2020). Core curriculum for the hospice and palliative APRN (Third, Vol. 2). Hospice And Palliative Nurses Association.


